INTRODUCTION
Patients with oral anticoagulation therapy (OAT) with vitamin K antagonists (VKA) undergo invasive procedures. Deciding wether to withdraw or maintain the OAT, as well as the needing to implement low molecular weight heparin (LMWH) as bridge therapy (BT), will be determined by the patient's thrombotic risk (TR) and surgery’s haemorrhagic risk (HR).
Patients with oral anticoagulation therapy (OAT) with vitamin K antagonists (VKA) undergo invasive procedures. Deciding wether to withdraw or maintain the OAT, as well as the needing to implement low molecular weight heparin (LMWH) as bridge therapy (BT), will be determined by the patient's thrombotic risk (TR) and surgery’s haemorrhagic risk (HR).
OBJECTIVE
To decrease bleeding events related to surgery by limiting the use of LMWH with patients having high TR.
To decrease bleeding events related to surgery by limiting the use of LMWH with patients having high TR.
METHOD
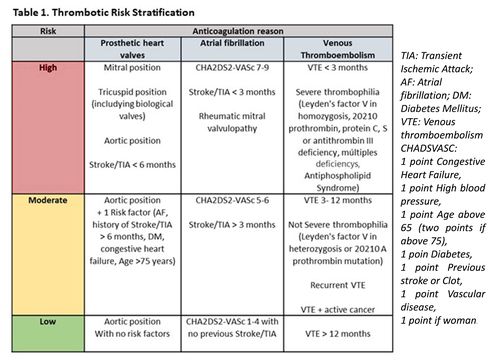
Prospective, unicentric, observational study including 200 patients with OAT undergoing surgery (December2019-February2021), with a follow-up of 4 weeks. The median age is 73 (33-93). Most patients are low TR on CHADs-VASc score. Periprocedural management of OAT was in accordance with the approved hospital protocol which classifies patients according to TR (Table1) and surgeries according to HR. VKA is suspended 3 days before surgery and resumed 24 hours after. LMWH as BT is reserved for patients with high TR or suspected active cancer (therapeutic dose), starting with OAT suspension and reintroduced along with it 24 hours after surgery for 3 days (if no bleeding complications).
Prospective, unicentric, observational study including 200 patients with OAT undergoing surgery (December2019-February2021), with a follow-up of 4 weeks. The median age is 73 (33-93). Most patients are low TR on CHADs-VASc score. Periprocedural management of OAT was in accordance with the approved hospital protocol which classifies patients according to TR (Table1) and surgeries according to HR. VKA is suspended 3 days before surgery and resumed 24 hours after. LMWH as BT is reserved for patients with high TR or suspected active cancer (therapeutic dose), starting with OAT suspension and reintroduced along with it 24 hours after surgery for 3 days (if no bleeding complications).
RESULTS
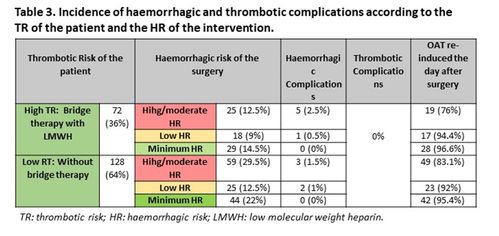
Interventions and clinical events during the follow-up are shown in Table 2.Eleven post-surgical haemorrhagicevents (5,5%) are described[GJ1] . Three (two hemoperitoneumand one haematomaof anterior rectus abdominis muscle) required hospitalisationfor management, being solved with conservative treatment. Eight were mild events, handled outpatiently. No thrombotic events were recorded. Generally, OAT was re-induced the day after surgery in patients undergoing minimal and low HR interventions, being the percentage lower in patients undergoing high HR interventions
Interventions and clinical events during the follow-up are shown in Table 2.Eleven post-surgical haemorrhagicevents (5,5%) are described[GJ1] . Three (two hemoperitoneumand one haematomaof anterior rectus abdominis muscle) required hospitalisationfor management, being solved with conservative treatment. Eight were mild events, handled outpatiently. No thrombotic events were recorded. Generally, OAT was re-induced the day after surgery in patients undergoing minimal and low HR interventions, being the percentage lower in patients undergoing high HR interventions
CONCLUSION
The standardization of periproceduralmanagement protocol for OAT adjusting BT with LMWH according to individual risk factors for each patient resulted in a reduction in the incidence of haemorrhagiccomplications without secondary increase of thromboembolic events. This study demonstrates the importance of a central, unified periproceduralmanagement protocol.
The standardization of periproceduralmanagement protocol for OAT adjusting BT with LMWH according to individual risk factors for each patient resulted in a reduction in the incidence of haemorrhagiccomplications without secondary increase of thromboembolic events. This study demonstrates the importance of a central, unified periproceduralmanagement protocol.
REFERENCES
- James D. Douketis, M.D., Alex C. Spyropoulos, M.D., ET. Al. erioperativeBridging Anticoagulation in Patients with Atrial Fibrillation. August27, 2015. N EnglJ Med2015; 373:823-833
- Protocolo de manejo perioperatoriode anticoagulación Hospital Universitario Príncipe de Asturias, Abril 2019.
- Vivas D, et al. Manejo perioperatorioy periprocedimientodel tratamiento antitrombótico: documento de consenso de SEC, SEDAR, SEACV, SECTCV, AEC, SECPRE, SEPD, SEGO, SEHH, SETH, SEMERGEN, SEMFYC, SEMG, SEMICYUC, SEMI, SEMES, SEPAR, SENEC, SEO, SEPA, SERVEI, SECOT y AEU.RevEspCardiol. 2018.
The data in this poster was presented at EHA 2021. Published with permission from the Copyright owner.
