1Hematología, Hospital Universitario de Salamanca
ABSTRACT
Haploidentical HLA stem cell transplantation (haplo-HSCT) is increasingly being used as part of the treatment of hematological malignancies lacking a suitable HLA-matched donor. Cytokine release syndrome (CRS) has been described in haplo-HSCT, but its clinical impact on these patients is controversial.In order to identify novel CRS features that might have a prognostic impact on haplo-HSCT, retrospective data from 51 patients receiving peripheral blood haplo-HSCT in 2019 and 2020 in our centre was analyzed.The median age was 51 years (range 17-72), 59% were male. Median follow-up was 359 days for alive patients. 84% of the patients presented with CRS after haplo-HSCT (71% of them occurred in the first 48 hours after infusion). CRS was mild in most patients: grade 1 in 29 (71%) and grade 2 in 12 (29%); no grade 3 CRS or further occurred. Graft cryopreservation accounted for 13 (25%) patients.Early-onset CRS (<48h since stem cell infusion) was associated with lower overall survival (p=0,01), as well as lower event free survival (relapse or death, p=0,03) when compared with the remaining patients in a univariate analysis.Although this is a retrospective single-centre analysis, it might provide new insights about the relevance of CRS in haplo-HSCT.
Haploidentical HLA stem cell transplantation (haplo-HSCT) is increasingly being used as part of the treatment of hematological malignancies lacking a suitable HLA-matched donor. Cytokine release syndrome (CRS) has been described in haplo-HSCT, but its clinical impact on these patients is controversial.In order to identify novel CRS features that might have a prognostic impact on haplo-HSCT, retrospective data from 51 patients receiving peripheral blood haplo-HSCT in 2019 and 2020 in our centre was analyzed.The median age was 51 years (range 17-72), 59% were male. Median follow-up was 359 days for alive patients. 84% of the patients presented with CRS after haplo-HSCT (71% of them occurred in the first 48 hours after infusion). CRS was mild in most patients: grade 1 in 29 (71%) and grade 2 in 12 (29%); no grade 3 CRS or further occurred. Graft cryopreservation accounted for 13 (25%) patients.Early-onset CRS (<48h since stem cell infusion) was associated with lower overall survival (p=0,01), as well as lower event free survival (relapse or death, p=0,03) when compared with the remaining patients in a univariate analysis.Although this is a retrospective single-centre analysis, it might provide new insights about the relevance of CRS in haplo-HSCT.
INTRODUCTION
Haploidentical HLA stem cell transplantation (haplo-HSCT) is increasingly being used as part of the treatment of hematological malignancies lacking a suitable HLA-matched donor.Cytokine release syndrome (CRS) is a systemic inflammatory response with aberrant immune activation and hyperstimulation which has been described in a number of clinical settings, including haplo-HSCT. However, clinical impact of CRS on these patients is controversial.During COVID-19 pandemic, graft cryopreservation in haplo-HSCT has increased in our centre. As a result, we clinically noticed a change in CRS onset in these patients.
Haploidentical HLA stem cell transplantation (haplo-HSCT) is increasingly being used as part of the treatment of hematological malignancies lacking a suitable HLA-matched donor.Cytokine release syndrome (CRS) is a systemic inflammatory response with aberrant immune activation and hyperstimulation which has been described in a number of clinical settings, including haplo-HSCT. However, clinical impact of CRS on these patients is controversial.During COVID-19 pandemic, graft cryopreservation in haplo-HSCT has increased in our centre. As a result, we clinically noticed a change in CRS onset in these patients.
METHOD
A cohort of 154 patients undergoing allogeneic stem cell transplantation in 2019 and 2020 in our centre, from which 51 patients receiving peripheral blood haplo-HSCT from 1st February 2019 to 31st December 2020 were selected. Two of them were excluded for the CRS analysis due to relevant microbiological isolation close to the infusion date and impossibility to distinguish between infectious and CRS fever. CRS was graded according to the ASBMT consensus[1].
A cohort of 154 patients undergoing allogeneic stem cell transplantation in 2019 and 2020 in our centre, from which 51 patients receiving peripheral blood haplo-HSCT from 1st February 2019 to 31st December 2020 were selected. Two of them were excluded for the CRS analysis due to relevant microbiological isolation close to the infusion date and impossibility to distinguish between infectious and CRS fever. CRS was graded according to the ASBMT consensus[1].
RESULT
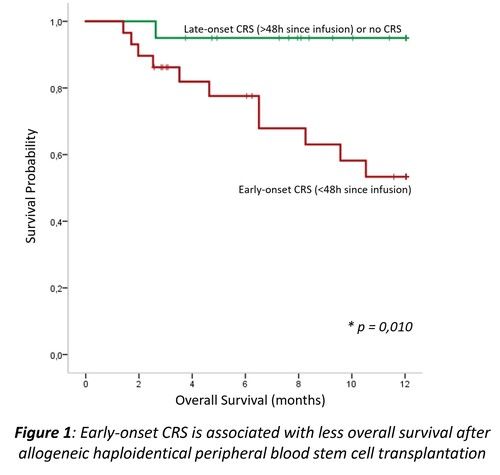
The median age was 51 years (range 17-72), 59% were male.Median follow-up was 359daysfor alive patients.Hematopoietic Cell Transplantation Comorbidity Index (HCT-CI) was low risk in 45%, intermediate risk in 22% and high risk in 33%. Most patients (71%) had an intermediate Disease Risk Index (DRI). Conditioning regimen was myeloablative in 12 (24%). 84% of the patients presented with CRS after haplo-HSCT(71% of them occurred in the first 48 hours after infusion). CRS was mild in most patients (grade 1 in 29 (71%) and grade 2 in 12 (29%); no grade 3 CRS or further occurred. Graft cryopreservation accounted for 13 (25%)patients.Baseline patient characteristics from our cohort are summarizedin Table 1.Early-onset CRS (<48h since stem cell infusion) was associated with loweroverall survival(Figure 1,p=0,01),as well as lowerevent free survival(relapse or death,p=0,03)when compared with the remaining patients in a univariate analysis.Non-myeloablative conditioning was associated with a higher proportion of early-onset CRS, which could be related to different immunossuppresion platform, as we also found higher proportion of early-onset CRS with modified Baltimore platform (starting both tacrolimus and mycophenolate on day +5 and administering cyclophosphamide on days +3 and +4[2]) when compared to Raiola platform(starting calcineurin inhibitor on day 0, mycophenolateon +1 and administering cyclophosphamide on days +3 and +5[3]), regardless of conditioning regimen.Age >60 years was also associated with a higher proportion of early-onset CRS (80% vs 45% p=0,014)and itshould be noted that age>60 yearsdid not impact on overall survival in the first year following haplo-HSCTin our patients (p=0,485).We alsofound an interesting trend between graft cryopreservation and early-onset CRS(only 38% of patients with graft cryopreservation presented early-onset CRS, whereas 67% of patients with fresh graft did so,p=0,075).Cryopreservation was related to less proportion of CRS grade≥2(0% vs 33%,p=0,014) and it did not impact on engraftment, overall survival nor graft versus receptor disease rate or severityin our patients. Patients with refractory disease prior to transplantation presented higher rates of CRS grade ≥2 (75% vs 20%,p=0,041). Moreover, a trend was observed for mononucleated cell count >8 x 108(37% vs 14%,p=0,067). However, CRS grade ≥2 did not impactonoverall survival in our patients (p=0,251).Variables associated with developing early-onset CRS following haplo-HSCT in our patients are summarized in Table 2.
The median age was 51 years (range 17-72), 59% were male.Median follow-up was 359daysfor alive patients.Hematopoietic Cell Transplantation Comorbidity Index (HCT-CI) was low risk in 45%, intermediate risk in 22% and high risk in 33%. Most patients (71%) had an intermediate Disease Risk Index (DRI). Conditioning regimen was myeloablative in 12 (24%). 84% of the patients presented with CRS after haplo-HSCT(71% of them occurred in the first 48 hours after infusion). CRS was mild in most patients (grade 1 in 29 (71%) and grade 2 in 12 (29%); no grade 3 CRS or further occurred. Graft cryopreservation accounted for 13 (25%)patients.Baseline patient characteristics from our cohort are summarizedin Table 1.Early-onset CRS (<48h since stem cell infusion) was associated with loweroverall survival(Figure 1,p=0,01),as well as lowerevent free survival(relapse or death,p=0,03)when compared with the remaining patients in a univariate analysis.Non-myeloablative conditioning was associated with a higher proportion of early-onset CRS, which could be related to different immunossuppresion platform, as we also found higher proportion of early-onset CRS with modified Baltimore platform (starting both tacrolimus and mycophenolate on day +5 and administering cyclophosphamide on days +3 and +4[2]) when compared to Raiola platform(starting calcineurin inhibitor on day 0, mycophenolateon +1 and administering cyclophosphamide on days +3 and +5[3]), regardless of conditioning regimen.Age >60 years was also associated with a higher proportion of early-onset CRS (80% vs 45% p=0,014)and itshould be noted that age>60 yearsdid not impact on overall survival in the first year following haplo-HSCTin our patients (p=0,485).We alsofound an interesting trend between graft cryopreservation and early-onset CRS(only 38% of patients with graft cryopreservation presented early-onset CRS, whereas 67% of patients with fresh graft did so,p=0,075).Cryopreservation was related to less proportion of CRS grade≥2(0% vs 33%,p=0,014) and it did not impact on engraftment, overall survival nor graft versus receptor disease rate or severityin our patients. Patients with refractory disease prior to transplantation presented higher rates of CRS grade ≥2 (75% vs 20%,p=0,041). Moreover, a trend was observed for mononucleated cell count >8 x 108(37% vs 14%,p=0,067). However, CRS grade ≥2 did not impactonoverall survival in our patients (p=0,251).Variables associated with developing early-onset CRS following haplo-HSCT in our patients are summarized in Table 2.
Figure 1
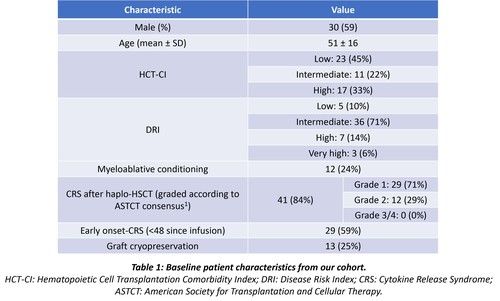
Figure 2
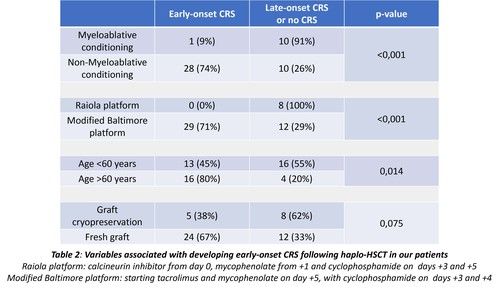
Figure 3
CONCLUSION
Early-onset CRS is associatedwith less overall survival and less event-free survival following the first year after haplo-HSCT. Cryopreservation is associated with less CRS grade≥2 probability and might also reduce the chance of developing early-onset CRS. Although this is a retrospective single-centre analysis, it might provide new insights about the relevance of CRS in haplo-HSCT.
Early-onset CRS is associatedwith less overall survival and less event-free survival following the first year after haplo-HSCT. Cryopreservation is associated with less CRS grade≥2 probability and might also reduce the chance of developing early-onset CRS. Although this is a retrospective single-centre analysis, it might provide new insights about the relevance of CRS in haplo-HSCT.
REFERENCES
1 Lee DW et al. ASTCT Consensus Grading for Cytokine Release Syndrome and Neurologic Toxicity Associated with Immune Effector Cells. Biol Blood Marrow Transplant 2019; 25(4): 625-38.
2 Luznik L et al. HLA-haploidentical bone marrow transplantation for hematologic malignancies using nonmyeloablative conditioning and high-dose, posttransplantation cyclophosphamide. Biol Blood Marrow Transplant. 2008;14(6):641–50.
3 Raiola AM et al. Unmanipulated haploidentical bone marrow transplantation and posttransplantation cyclophosphamide for hematologic malignancies after myeloablative conditioning. Biol Blood Marrow Transplant. 2013;19(1):117–22.
1 Lee DW et al. ASTCT Consensus Grading for Cytokine Release Syndrome and Neurologic Toxicity Associated with Immune Effector Cells. Biol Blood Marrow Transplant 2019; 25(4): 625-38.
2 Luznik L et al. HLA-haploidentical bone marrow transplantation for hematologic malignancies using nonmyeloablative conditioning and high-dose, posttransplantation cyclophosphamide. Biol Blood Marrow Transplant. 2008;14(6):641–50.
3 Raiola AM et al. Unmanipulated haploidentical bone marrow transplantation and posttransplantation cyclophosphamide for hematologic malignancies after myeloablative conditioning. Biol Blood Marrow Transplant. 2013;19(1):117–22.
The data in this poster was presented at EHA 2021. Published with permission from the Copyright owner.
