INTRODUCTION
The impact of pretransplant body mass index (BMI) on outcomes of allogeneic stem cell transplantation (ASCT) Is still controversial. Most studies reported that pretransplant obesity was associated with lower survival [1-3]. However other authors reported that patients with BMI>23 kg/m 2 had an increased overall survival (OS) compared to those with lower BMI [4], while others concluded that BMI did not impact ASCT outcomes [5].
The aim of this study is to evaluate the impact of pretransplant BMI on transplant related complications and survival.
The impact of pretransplant body mass index (BMI) on outcomes of allogeneic stem cell transplantation (ASCT) Is still controversial. Most studies reported that pretransplant obesity was associated with lower survival [1-3]. However other authors reported that patients with BMI>23 kg/m 2 had an increased overall survival (OS) compared to those with lower BMI [4], while others concluded that BMI did not impact ASCT outcomes [5].
The aim of this study is to evaluate the impact of pretransplant BMI on transplant related complications and survival.
MATERIALS AND METHODS
We performed a retrospective study on patients who underwent ASCT from HLA-identical sibling donors between June 2015 and December 2018. Conditioning regimen consisted of Busulfex and Cyclophosphamide (Bu/Cy) or Fludarabine and Busulfex (Flud/Bu) in myeloid malignancies, TBI or thiotepa-based regimen in Lymphoid malignancies and antithymoglobuline (ATG) and cyclophosphamide with or without fludarabine in aplastic anemia. Graft-versus host disease (GVHD) prophylaxis consisted of cyclosporine and short course of methotrexate.
Patients were stratified according to pretransplant BMI values defined by the World Health Organization: underweight (BMI<18 kg/m2), normal BMI (18-25kg/m2), overweight (BMI 25-30 kg/m2) and obese (BMI>30 kg/m2).
We performed a retrospective study on patients who underwent ASCT from HLA-identical sibling donors between June 2015 and December 2018. Conditioning regimen consisted of Busulfex and Cyclophosphamide (Bu/Cy) or Fludarabine and Busulfex (Flud/Bu) in myeloid malignancies, TBI or thiotepa-based regimen in Lymphoid malignancies and antithymoglobuline (ATG) and cyclophosphamide with or without fludarabine in aplastic anemia. Graft-versus host disease (GVHD) prophylaxis consisted of cyclosporine and short course of methotrexate.
Patients were stratified according to pretransplant BMI values defined by the World Health Organization: underweight (BMI<18 kg/m2), normal BMI (18-25kg/m2), overweight (BMI 25-30 kg/m2) and obese (BMI>30 kg/m2).
RESULTS AND DISCUSSION
One hundred and nineteen patients were included (71 males and 48 females). The median age was 34 years (range, 7- 49y). Diseases were acute myeloid leukemia (n=37, 31%), acute lymphoblastic leukemia (n=31, 26%), aplastic anemia (n=27, 22.7%), chronic myeloid leukemia or myeloproliferative neoplasms (n=16, 13,5%), myelodysplastic syndrome (n=4, 3.4%) and non- Hodgkin’s lymphoma (n=4, 3.4%). According to the pretransplant BMI values, 45% of patients have a normal BMI, 13% were obese, 24% were in overweight and 18% were in underweight. The characteristics of four groups are summarized in Table 1.
There was no statistically significant association between pretransplant BMI and incidence of acute or chronic GVHD, acute infectious complications and relapse rate (p=0.74, p=0.15 and p=0.93, respectively). After a median follow-up of 20 months (range, 4-54 months), the OS, RFS and NRM in the whole cohort were 76.8%, 53% and 12.5%, respectively.
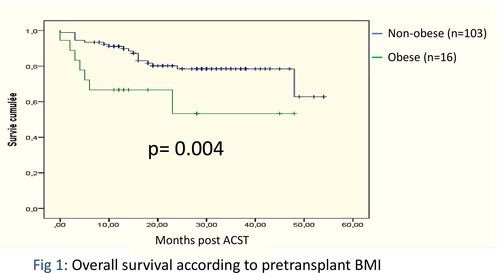
Obese patients have a significantly lower OS compared with other patients (78% vs92%, p=0.004, respectively) (figure 1). The RFS and the NRM were not statistically different between obese and non-obese patients (p=0.37 and p=0.7, respectively).
In our study, obesity impacted negatively the OS compared to non-obese patients. NRM was the main cause of death among these patients (6/7). One of the possible reasons is that obese patients possibly had higher cumulative drug doses or longer drug exposure times especially for lipophilic drugs (Busulfan and cyclophosphamide) [4]. Half of the obese patients received these drugs in our study.
The largest study on the impact of pretransplant BMI after ASCT showed that underweight patients had worse OS due to the increased risk of relapse and obese patients had increased NRM do to the higher incidences of hepatic and gut acute GVHD in comparison with patients with normal BMI [6]. The hematopoietic cell transplantation specific comorbidity index classifies also obesity as a negative risk factor for NRM [7].
One hundred and nineteen patients were included (71 males and 48 females). The median age was 34 years (range, 7- 49y). Diseases were acute myeloid leukemia (n=37, 31%), acute lymphoblastic leukemia (n=31, 26%), aplastic anemia (n=27, 22.7%), chronic myeloid leukemia or myeloproliferative neoplasms (n=16, 13,5%), myelodysplastic syndrome (n=4, 3.4%) and non- Hodgkin’s lymphoma (n=4, 3.4%). According to the pretransplant BMI values, 45% of patients have a normal BMI, 13% were obese, 24% were in overweight and 18% were in underweight. The characteristics of four groups are summarized in Table 1.
There was no statistically significant association between pretransplant BMI and incidence of acute or chronic GVHD, acute infectious complications and relapse rate (p=0.74, p=0.15 and p=0.93, respectively). After a median follow-up of 20 months (range, 4-54 months), the OS, RFS and NRM in the whole cohort were 76.8%, 53% and 12.5%, respectively.
Obese patients have a significantly lower OS compared with other patients (78% vs92%, p=0.004, respectively) (figure 1). The RFS and the NRM were not statistically different between obese and non-obese patients (p=0.37 and p=0.7, respectively).
In our study, obesity impacted negatively the OS compared to non-obese patients. NRM was the main cause of death among these patients (6/7). One of the possible reasons is that obese patients possibly had higher cumulative drug doses or longer drug exposure times especially for lipophilic drugs (Busulfan and cyclophosphamide) [4]. Half of the obese patients received these drugs in our study.
The largest study on the impact of pretransplant BMI after ASCT showed that underweight patients had worse OS due to the increased risk of relapse and obese patients had increased NRM do to the higher incidences of hepatic and gut acute GVHD in comparison with patients with normal BMI [6]. The hematopoietic cell transplantation specific comorbidity index classifies also obesity as a negative risk factor for NRM [7].
CONCLUSIONS
Pretransplant obesity was associated with inferior OS after ASCT without impacting treatment related complications. A prospective study with multivariate analysis is needed to better identify the impact of BMI on allogeneic transplant outcomes.
Pretransplant obesity was associated with inferior OS after ASCT without impacting treatment related complications. A prospective study with multivariate analysis is needed to better identify the impact of BMI on allogeneic transplant outcomes.
Figure 1
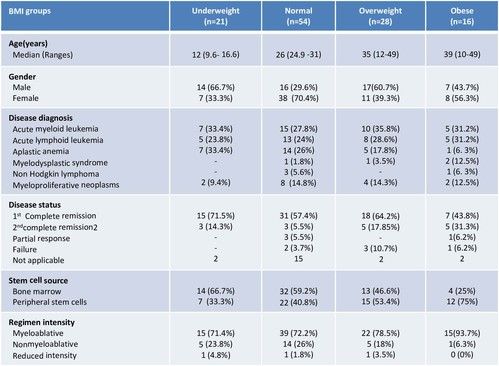
Figure 2
FUNDING STATEMENT
Centre National de Greffe de Moelle osseuse de Tunis, Tunisia
REFERENCES
1. Fuji S, Kim S, Yoshimura K, Akiyama H, Okamoto S, Sao H, et al. Possible association
between obesity and post-transplantation complications including infectious diseases
and acute graft-versus-host disease. Biol blood marrow transpl. 2009;15:73–82.
2. Nakao M, Chihara D, Niimi A, Ueda R, Tanaka H, Morishima Y, et al. Impact of being
overweight on outcomes of hematopoietic sct: a meta-analysis. Bone marrow
transplant. 2013;49:66–72.
3. Weiss BM, Vogl DT, Berger NA, Stadtmauer EA, Lazarus HM. Trimming the fat:
obesity and hematopoietic cell transplantation. bone marrow transplant.
2012;48:1152–60.
4. Yang J, Xue SL, Zhang X, Zhou YN, Qin LQ, Shen YP, Wu DP. Effect of body mass index
on overall survival of patients with allogeneic hematopoietic stem cell
transplantation. European Journal of Clinical Nutrition (2017) 71, 750–754.
5. Nikolousis E, Nagra S, Paneesha S, Delgado J, Holder K, Bratby L et al. Allogeneic
transplant outcomes are not affected by body mass index (BMI) in patients with
haematological malignancies. Ann Hematol 2010; 89: 1141–1145.
6. Fuji S, Takano K, Mori T, Eto T, Taniguchi S, Ohashi K, et al. Impact of pre-transplant
body mass index on the clinical outcomes after allogeneic hematopoietic SCT. Bone
Marrow Transplant. 2014;49:1505–12 .
7. Sorror ML, Maris MB, Storb R, Baron F, Sandmaier BM, Maloney DG, et al.
Hematopoietic cell transplantation (HCT)- specific comorbidity index: a new tool for
risk assessment before allogeneic HCT. Blood. 2005;106:2912–9.
The data in this poster was presented at EHA 2021. Published with permission from the Copyright owner.
